Our Perspective
Enough is enough.
Rampant medical billing abuse hurts everyone. WellRithms was founded to relieve the financial and emotional stress caused by a broken healthcare system. By identifying and eliminating billing waste, we help payors including fiduciaries, employers, carriers, and claims administrators protect resources and deliver fair outcomes.
Who We Serve
THE ONE WHO PICKS UP THE TAB
From Group Health to Workers’ Comp to Auto, Every Payor Deserves Better
Group Health Plans
Expertly serving Self-Funded Employers, Union Trusts, Brokers & Consultants, and TPAs, revolutionizing healthcare billing across diverse industry markets.
Comp42: Advanced Payment Integrity for Complex Workers’ Comp Claims
Introducing Comp42, our data-driven workers’ comp payment integrity suite. Leveraging advanced analytics, physician-led validation, and defensible reimbursement methodologies, Comp42 protects payors from volatility across high-severity claims.

Auto Casualty Solutions
Bill review companies and auto payors work in tandem with WellRithms to curb the uncertainties of casualty billing by providing additional layers of payment integrity and deeper bill analysis.
Why WellRithms
Key Differentiators
Automation alone cannot resolve high-complexity claims. Flagged and high-exposure cases are reviewed by physicians and surgeons who understand the medicine behind the billing. This clinical depth ensures appropriate reimbursement decisions grounded in medical reality, not coding convention alone.
Our reimbursement methodologies are grounded in hospital cost data and transparent cost-plus models. Unlike outdated multiples of Medicare, our approach produces payment positions that are fair, sustainable, and legally defensible across all the markets we serve.
With more than 25 years of experience defending reimbursement positions in courts nationwide, WellRithms has helped establish legal precedent supporting fair and reasonable payment methodologies. Our approach is built not only for savings, but for defensibility under scrutiny.
Through WellRithms Shield Indemnification™ and our captive structure, we align with payors by assuming defined financial risk on disputed claims. This framework reduces financial volatility while reinforcing confidence in our payment integrity methodology.
Shield Indemnification™
Guaranteeing our recommended payment amount
Shield Indemnification™ protects carriers, plans, and members from the adverse impact of litigation expenses and balance billing tactics.
We are backed by a captive insurance company that allows for the transfer of all legal and financial liability from the payor to WellRithms, thereby guaranteeing the recommended payment amount.
Client Testimonials
HEAR FROM OUR CLIENTS
Discover how WellRithms has transformed healthcare reimbursement for our clients. Read firsthand accounts of our success stories striving to deliver precise, fair, and effective solutions.
“I cannot express my gratitude for the advocacy and guidance that this organization fosters. The timing of the original bill came at the worst possible time for me and my family, financially, and we are grateful beyond measure. It was an amazing feeling through it all, to know someone had my back!”
“WellRithms helped me so much when medical companies were bullying me and sending bills out of nowhere years after the incident. SO grateful for them.”
“I immediately felt relieved and like I was in good hands when I contacted WellRithms for help with some medical bills I’d incurred. They were so attentive, reassuring, and kind, that I wasn’t at all surprised when they successfully reduced my debt considerably.”
“You guys are slowly slaying the dragon. I’ve heard nothing [from collections]. They’re afraid of you! Who are you guys? A secret league of crimefighters?? Thanks so much again!”
“We have not received anything at this time [from collections]. Thank you for everything. You’re a godsend!”
“…the indemnification part seemed too good to be true…but ultimately, I decided to do it. It’s the best decision I’ve ever made.”
“No one’s ever contacted me again. Many people have asked me what this company did for me…They waved some sort of magic wand. That’s what it feels like.”
“The entire process was amazing. You checked in every month, and when you weren’t working on the case anymore, someone else continued to do that. I felt like I got explanations every step of the way. It was seamless.”
“It was a great experience, and I’m glad that you exist.”
“…for the first time in months, I had hope that there was a potential resolution. So, I can’t thank you guys enough, it was a great experience, and I’m glad that you exist.”
Subscribe to Our Newsletter

Featured Insights
Proposed by Congress. Proven by WellRithms.
Blog
The National Healthcare Conversation Is Changing. Our Approach Hasn’t. Across the United States, policymakers are reexamining how healthcare dollars move through…
Exposing Trauma Response Charges
Bill of the Month
A California-based hospital recently submitted a bill of $100,618 for a one-night stay, all centered around a treatment for a fractured…
Medical Overbilling: Examining the Heart of the Problem
Bill of the Month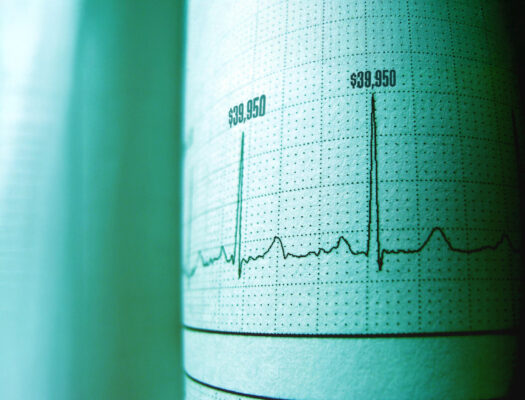
A two-day hospital stay in a California-based hospital gave our bill review team some serious heart palpitations – not from medical…
WellRithms Recognized as a Rising Star in BenefitsPRO’s 2024 Luminaries Awards
BlogWe are honored that WellRithms has been named to BenefitsPRO Luminaries Class of 2024 in the Rising Star category. This recognition…
WellRithms Launches Comp42
Media
PORTLAND, Ore., Oct. 15, 2024 (GLOBE NEWSWIRE) — WellRithms, the industry leading payment integrity firm, demonstrates its market leadership with the launch…
WellRithms Unveils Comp42: Revolutionizing Workers’ Compensation Bill Review
BlogAt the forefront of payment integrity, WellRithms has launched Comp42, a groundbreaking solution designed to tackle one of the most pervasive…
Member Support
Find out answers to any questions you have with your account.
Want to Know More?
See how WellRithms addresses the problem of billing errors, waste, abuse and potential fraud.
