There are BILLIONS of reasons to fight healthcare overbilling
Million-dollar claims are more and more frequent. Outpatient procedures commonly exceed $50,000. Inpatient procedures frequently exceed $100,000. Payors and administrators lack supporting documentation to really understand the bill.
WellRithms integrates with the claims administration process to ensure that every bill is cleaned of errors, accurately priced, and consistent with the care received.

A Year
That’s the average cost of family health benefits coverage, including employee contribution.

Innovative Solutions
Experience Guaranteed Savings
WellRithms Is the Solution for Accurate Medical Claim Review and Repricing
In-Network Impact
Classification, Edits, & Review™
- Network claims are reviewed line-by-line using WellRithms’ Classification, Edits, & Review (CER) system, before PPO discount is applied.
Inpatient Itemized Bill Review
- Automated Line-by-Line review. Amplifying the review process by automating data extraction from imaged itemized bills and mapping them into our system.

Out-of-Network Impact
Sustainable Claims Pricing™ (SCP)
- Revolutionizing the way out-of-network and catastrophic healthcare bills are adjudicated.
Air / Ground Ambulance Repricing
- Ensures the accuracy and integrity of medical bills before payment.
RBP Cleanup
RBP Cleanup
- Ensuring disputes are resolved with accuracy and fairness, backed by full legal and financial support.

Shield Indemnification™
Guaranteeing our recommended payment amount
Shield Indemnification™ protects carriers, plans, and members from the adverse impact of litigation expenses and balance billing tactics.
We are backed by a captive insurance company that allows for the transfer of all legal and financial liability from the payor to WellRithms, thereby guaranteeing the recommended payment amount.
Featured Insights
Proposed by Congress. Proven by WellRithms.
Blog
The National Healthcare Conversation Is Changing. Our Approach Hasn’t. Across the United States, policymakers are reexamining how healthcare dollars move through…
Exposing Trauma Response Charges
Bill of the Month
A California-based hospital recently submitted a bill of $100,618 for a one-night stay, all centered around a treatment for a fractured…
Medical Overbilling: Examining the Heart of the Problem
Bill of the Month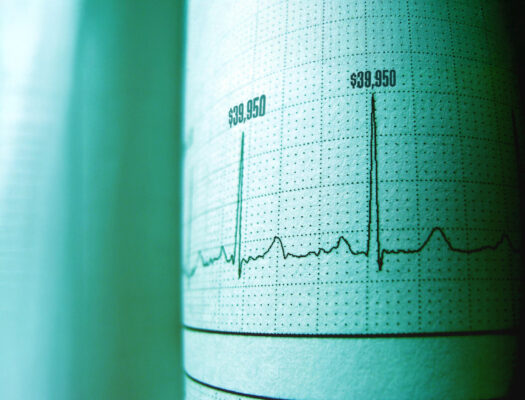
A two-day hospital stay in a California-based hospital gave our bill review team some serious heart palpitations – not from medical…
Member Support
Find out answers to any questions you have with your account.
Group Health Provider Inquiries
Find out answers to any questions you have.