Insights
Blog
WellRithms Recognized as a Rising Star in BenefitsPRO’s 2024 Luminaries Awards
We are honored that WellRithms has been named to BenefitsPRO Luminaries Class of 2024 in the Rising Star category. This recognition…
WellRithms Unveils Comp42: Revolutionizing Workers’ Compensation Bill Review
At the forefront of payment integrity, WellRithms has launched Comp42, a groundbreaking solution designed to tackle one of the most pervasive…
Expanding Our Leadership: Key Appointments at WellRithms

We’re thrilled to announce important leadership changes and promotions as we continue our growth and innovation. These strategic appointments reflect our…
Media
WellRithms Launches Comp42

PORTLAND, Ore., Oct. 15, 2024 (GLOBE NEWSWIRE) — WellRithms, the industry leading payment integrity firm, demonstrates its market leadership with the launch…
WellRithms and Blackwell Captive Announce Collaboration

CHICAGO and PORTLAND, Ore., Sept. 17, 2024 (GLOBE NEWSWIRE) — Blackwell Captive Solutions, a leading provider of innovative captive solutions and WellRithms, the…
WellRithms Recognized Again for Rapid Growth

WellRithms Featured for Fourth Consecutive Year on Portland Business Journal List of Fastest-Growing Private Companies September 16, 2024 10:00 ET |…
Bill of the Month
Medical Overbilling: Examining the Heart of the Problem
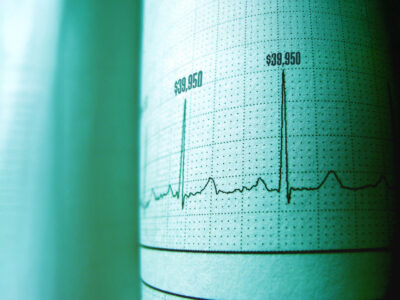
A two-day hospital stay in a California-based hospital gave our bill review team some serious heart palpitations – not from medical…
Addressing Overpriced Medical Imaging Bill in Workers’ Compensation Case

Certain health care services are expensive, but some bills take pricing to a whole new level. This was the case for…
Slashing Overpriced Bills for Newborn Care Preserves ‘Piggy Bank’ Savings

When an underweight newborn struggled with feeding, the baby was admitted to the Level II Neonatal Special Care Nursery at Doctors…
Proven Results
Down-and-Out in Beverly Hills: How a Hernia Repair Mirrors Larger Problems
Healthcare costs vary wildly depending on where you are, sometimes even within the same neighborhood. This disparity, often overlooked, fuels a…
How WellRithms Kept One Customer from Footing an Egregious Podiatry Bill

In our line of work, we always come across egregious billing practices – some worse than others. But few were as…
The Audacity to Sue
A 6-year-old girl fell and cut her ankle open a half-inch. Her mother sought treatment at an Out-of-Network clinic due to…
Get insights in your inbox
Sign up to our newsletter to stay up to date with latest WellRithms insights.

